
Medical procedures
• Shoulder replacements
• Sling Accessories
• Knees
• Back
My new bionic shoulders

Sometime in the spring of 2014, I was renovating the interior of my house - refinishing the floor, swapping out the corrugated tin and replacing it with rough cedar, and painting the walls a charcoal grey. I was reaching up to screw in the cedar planks and reaching up to paint the ceiling and upper walls. Ouch. Something hurt. I wasn't sure what it was, so I went on and just plowed through the pain. You know how guys are, "a little pain ain't gonna stop my work." The last section was painting the bedroom walls and ceiling. I could paint about a 3x3 foot section of ceiling before the pain got too great to continue. I would take a short break, lower my arms, and go back in to do another section. I had finished the rest of the house and wasn't going to let the pain stop me this close to finishing.
Oops, that machismo turned out to be quite damaging. A while later I saw an orthopedist who took x-rays and an MRI. There was a detached rotator cuff tendon, tears in the right rotator cuff and bicep, some arthritis, a bone spur, and loss of cartilage in the joint - that made a 'ratcheting' sound when I moved the arm.
We both wanted to avoid surgery so we tried some other options - Plasma Rich Platelet injections, Physical Therapy, and later, Stem Cell injections. Those attempts took about 2 years. There was some temporary relief.
In summer 2017, I experienced a flash of severe pain in my right arm and shoulder. I had re-torn something. Getting frustrated with the pain, I decided it was time for surgery. I had an MRI taken of the right shoulder and hand-delivered it to the Ortho office before my appt the next day. But, when I went in for the appt, they could not find the disk with the MRI. They acknowledged that they had received the disk and looked for it for about 30 minutes. Fortunately, by an earlier fluke, I had a second disk and drove that back to them that afternoon. Doc wanted to do another PRP injection. He prescribed medicine to take before the injection. At the pharmacy back in Edmond, I handed the scrip to the pharmacist who noted that it was a steroid and that I am not to take steroids due to the earlier stem cell injections. I drove back to the doctor in OKC (who knew I was not supposed to take any steroids) and they took back the prescription and told me just to take Aleve. There were several mistakes made by that office that afternoon (losing a disk, wrong prescription, not scheduling appts, incomplete PT prescrip.) I awoke the next morning with, "Jim, you're a fool if you trust your health to an office that makes major mistakes." I called another Orthopedist, at McBride, who had been recommended to me. I couldn't get in for about 2 weeks. Someone at my physical therapist's practice called and got me in in just two days. I took the MRI disk and a disk of x-rays to McBride. After a brief assessment, the PA started telling me what was going on inside my shoulder. I interrupted him asking, "Are you about to recommend surgery?" He paused, and said, "Yes."
"I'm ready, let's do it." We scheduled surgery right then for a date after my return from a previously scheduled trip to Santa Fe.


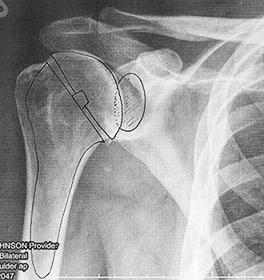
Right: The PA drew how the parts of the new shoulder would be placed. The large pieces on the left are the metal inserts. The bone is cut and removed and a hole drilled down into the bone marrow. The metal cone piece is inserted down into that hole. Then another metal piece - the dome-shaped cap - is attached to that piece. On the other side of the joint, the bone is ground away and a piece of plastic (the shaded oval above) is glued in place.
The shoulder was replaced with a metal and plastic version. While it may slow me down in the TSA line having to get wanded, it does mean I will never get arthritis in that shoulder. I stayed in the hospital for 3 days which was quite nice - somebody brought me food, somebody cleared the table, wearing pajamas all day was expected, and I could lay in bed and pee. I enjoyed talking with the nurses and with visitors who dropped by the room. The first few nights were rough as my body adjusted to the trauma of having bone cut out and all the accompanying tissues reattached. I'm such a wussy about blood and guts that I usually don't think about what went on inside that shoulder.
Before, when I moved my arm, there was this ratcheting tick and noise from the lack of cartilage, arthritis, and the bone spur. Now my shoulder moves Teflon smooth, absolutely silent, and with zero pain. It's wonderful.
Objectives
I have led quite a privileged and healthy life (I've only had a sprained ankle and minor knee pain that took care of itself). This would be my first surgery and first incision. I felt that it would help me connect and appreciate the many people that live with physical challenges & disabilities every day.
To aid healing and wellness, I wanted to meet these objectives:
• Enshroud the process in calmness, peace, and minimal stress (the 2 people I asked for rides to/from the hospital are the most calm and peaceful people I know).
• Maintain a positive attitude.
• Patiently cope with the physical challenges.
• Keep the shoulder immobile.
• Walk Brooklyn daily.
• Work a bit in the office each day.
• Exercise the right hand and forearm.
• Go to the gym for lower body exercises.
• Eat smart.


Timeline
Jan-Oct: House remodeling; shoulder pain, inflamed joint.
September 30: MRI left shoulder.
Fall: X-rays, steroids, Physical Therapy.
Oct 7: Platelet Rich Plasma procedure 1.
March 1: Stem cell & PRP procedure 2.
April-July: Physical Therapy.
May 2: PRP procedure 3.
June 28-July 1: Aggravated rotator cuff: intense shoulder/arm pain.
July/August: During the night, I would take Aleve to help me get through the morning waking hours, when the pain was its worst.
July 6: MRI right shoulder.
July 18: X-rays.
Switch orthopedists - saw McBride doctors.
July 21: Assessment with Brett and Matt; schedule surgery.
August 14-18: Enjoyed visiting friends in Santa Fe: Meow Wolf, the Opera, and hiking Bandelier.
August: Practiced daily life routines with just one hand .
August 25 FR: Pre-Op informational meeting.
August 26-27 SA/SU: bummer weekend, some anxiety, tried to stay positive.
August 28 MO: Felt eager to heal and move forward; saw surgery and recovery as a challenge (like many people face). Had a great day - I let negativity roll off and looked forward (should do that more). Will be inconvenienced, but I will deal with that. And it's only for a few weeks. That evening, I did the antiseptic shower/wipe routine, ate a bit at midnite, rinsed off, tried to sleep, some overnight pain.
• Total right shoulder replacement surgery, Part 1
McBride Orthopedic Hospital, Surgeon: Matt, Physician's Assistant: Brett
August 29 TU: The morning moved slow, packed a suitcase (that turned out to be unnecessary), and took Brooklyn to boarding. Melinda picked me up and drove me to the hospital. She gave me some great advice about staying ahead of the pain by taking meds regularly and on time. Checked in, completed paperwork, and settled into a Pre-Op room.
Pre-Op: the attending nurse asked how I was. "I'm nervous - I've never had surgery before and I'm not real sure what to expect." This woman then proceeded to reassure me and she explained each step of the day and what would happen. She was so appreciated. I relaxed some. Changed into that ridiculous "cover-up". Was already missing my clothes, my new shoes, and my phone pacifier.
Joanie visited, then I was knocked out cold; came to in my new room: tubed up, drugged, and wearing an arm sling. Ate crackers and Jello, drank Diet Coke for caffeine. Fascinated by my new environment. Had a good dinner, good drugs, good visits from friends, but poor sleep - worst night of the process - the nerve block injection wore off overnight and the body/mind sensed the trauma and pain - morphine helped a little bit.
August 30 WE: Started the pill routines. Moved to the chair for breakfast: omelet with cold brew coffee that Joanie brought. Surgeon Matt visited with update - there had been some complications (explained below). Physical Therapist helped me walk the hallway loop - twice. Had salmon and veggies for both lunch & dinner, made calls and texts. Visitors: Joanie, Mike.
August 31 TH: Nice sleep (but numerous interruptions), nice breakfast, nice nap; PT: a second walk-the-hallway routine. PA Brett visited for check-up and discharge details. Took a shower rinse, dressed in street clothes (who knew that would be so enjoyable?) Discharged from hospital; Gail & Rita took me to Sprouts and home for lunch. We got Brooklyn, home: nap. Okay sleep: with the arm sling, but it was comfortable enough.
September 1-4 Labor Day Weekend: Recluse, little movement, time to be still and heal.
First week: Would wake at about 3a. Instead of trying to go back to sleep, I just got up and started the day - relied on an afternoon nap to finish the night's sleep. I was fortunate that I could clear the calendar - very helpful to relieve any stress of appointments or having to look half decent during the day. Pain pills had a side effect of itching all over. Was eager to wean off of those meds. Visitors: Ruki, Patti, Joanie, Mike.
September 5 TU, 1-week post-surgery: Drove to store - first time driving and first time solo shopping. Returned to daily routine: breakfast while watching Jeopardy!, walked Brooklyn, etc.
September 7 TH evening: Nurse Sarah replaced dressing bandage 'Looks good, good surgeon, minimal scar.'
September 8 FR: Inspiration for Sling Accessories (more below).
September 8 FR evening: Drove to McBOH Emergency Room: swelling? bruising? Brett was on duty - said swelling & bruising were due to loss of blood and bicep surgery; suggested I wear the sling less.
September 8-9: Built and tested prototypes of Sling Accessories.
September 10 SU: Stopped prescription pain med Percocet, just Tylenol, wore sling less each day.
September 11 MO: Began doing almost-full routine of rehab exercises at Gold's Gym.
September 14 TH: Posted Sling Accessories webpage.
September 15 FR: Checkup, staples out.
September 16 SA evening: First night not wearing the sling to bed - slept much better.
September 18 MO: Physical Therapy: range of motion assessed - criteria already met; 2 more weeks to let the reattached bicep and rotator cuff heal.
September 22 FR: Bandages removed, neosporinned the scar. Put the sling away.
October 3 TU: Began full body routine of rehab exercises, soaked in the hotub.
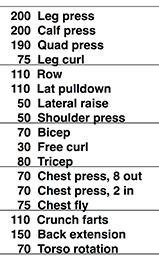
October 13 FR: 6 week checkup: Surgeon was impressed with the progress. I was way ahead of schedule with great range of motion. X-ray taken:
March 2 FR: 6 month checkup: PA was also pleased with the healing, range of motion, and strength.
July 13: Assessment of Left Shoulder.
August 31 FR: 1 year checkup: xray of right shoulder.
Febuary 22: Pre-Op informational meeting.
March 9-11: Practiced daily life routines with just right hand, prepped for surgery.
March 11 MO: Antiseptic shower/wipe routine, ate a bit at midnite, rinsed off, tried to sleep, some overnight pain.
• Total left shoulder replacement surgery, Part 2
McBride Orthopedic Hospital, Surgeon: Matt, Physician's Assistant: Brett
March 12 TU: Poor sleep, take Brooklyn to boarding, shower, Joanie pickup and drop off. Check-in, Pre-op: nerve block, out; surgery/post-op; Room 144, eat 7p: crackers peanut butter, tv, 11:15: crackers peanut butter, pudding, Started the pill routines.
March 13 WE: Matt visited with update (probly will go home today). Moved to the chair for breakfast: great omelet, cold brew coffee. Physical Therapist walk the hallway loop. Joanie visit. Bed: sleep. Lunch: salmon and veggies, coffee smoothie, PT walk, rest, changed cloze, got discharged nurse Stella. Joanie took me to get Brooklyn, food, and home: unpacked, set skeds for pills.
Days after surgery
0 Tube remove: oxygen (after surgery)
0 Tube remove: IV (evening of surgery)
1 Tube remove: drain (morning after surgery)
1 Tube remove: finger light (discharge after lunch)
3 Stop taking Percocet opioid
5 Drive to store
7 Sling off at home
"Yesterday the world looked great - I was in no pain and ready to get back to life. Overnight that changed. When the nerve block drugs wore off, the tremendous pain came back. I won’t be able to do anything today but drag my feet around the house. I feel miserable. It just came on last night like a blow from a sledge hammer - the feeling that I had been hit by a truck. And it was dark - I was having nightmares, bats in the deep dungeon of hell. Satan rode in on his red-eyed horse. And he does not like me - well I wasn’t real fond of him either. I was calling him names and I spit on him. I told him it was holy water. But it didn’t fool him, it just made him more angry and he shot at me with flames from under his fingernails. I realized I’ll have to repaint the bedroom - after I kick out the evil spirits and douse the flames in the lava that are oozing out of the electrical outlets."
March 14 TH: nightmares, nerve block wearing off, text cancel appts; FBI visit:
March 15 FR: Final Percocet: 1:30a, AFib morning.
March 17 SU: 2 walks, finish Lego, pm: first drive: maalox, fuzzys, tv.
March 18 MO: Poop day, chill inside, stomach quease.
March 19 TU: Shower, AppleStore, Doctor: change bandage, Target: sushi & ginger, rest, walk, Joanie Dramamine, dinner, rest.
March 20 WE: Panera lunch: Joanie play date, Mjok CrBl dinner, wore sling when out of home and overnight.
21-24 TH-SU: Rest, heal, order/install microwave, return house to normal.
March 26 TU: Began partial gym exercises, get/rebuild laptop.
March 29 FR: Checkup: staples out, bandage off, sling pillow away.
April 1-4 MO-TH: Train to Austin, Ft.Worth.
April 5 FR: Physical Therapy: range of motion assessed, exercises.
April 5 FR: First night not wearing the sling to bed - slept much better.
April 6 SA: Bandages fall off, neosporin & vitamin E the scar.
April 15 MO: Sling away, hotub.
April 16 TU: Began full body rehab exercises.
April 26 FR: 6+ week checkup. X-ray taken: all good.
June 14 FR: 3 month checkup: "You're all done."
June 18-July: Continued voluntary Physical Therapy.
Complications from 2017 surgery 1
Once I was opened up and the Surgeon and the PA were poking around, they discovered a strange mass - dried blood and bits of discarded cartilage had clumped together and attached to some of the bicep sinews.

Above: the dark oval is where blob of gunk was, the shaded triangle above and to the right is where some cartilage had been sloughed off and gathered on the bicep.
They vacuumed and picked out the pieces and removed the blob. I was not at all surprised to hear this as I had earlier experienced odd movements in the bicep accompanied by shooting bolts of pain. I had mentioned this to both orthopedists but they were at a loss as to what it was. Now we know. And it was taken care of. It shouldn't happen again as the parts are brand new and there are no longer the conditions (bone spur, arthritis, grinding) that caused it.
Maybe because of the extra time it took to remove that weird bicep thing, there was also a pretty large loss of blood. Not quite enough to warrant a transfusion, but enough that my body will be replenishing its pool of blood until sometime in late November. Getting lots of fresh blood sounds good, but I am now anemic and will experience some fatigue until then. Mornings are fine but by afternoon I'm pretty sluggish. But not bad - that just means I get to take a nap! Some days I don't even have much say in the matter. I lie down and I'm out.
When the incision was cauterized to help close the wound, a pad was adhered to the opposite-side thigh to ground the charge. In the hospital, I felt a strong surge of nerve pain where the pad was - my loud ouch brought in a nurse. At the time, I didn't know about the grounding pad - I naively thought it was due to the constriction hose on my legs. There were subsequent pain surges during the next few days and, for about 2 months, the thigh felt a bit numb with intermittent sharp pain.
Normally I am on my feet quite a bit and walk the dog twice a day. 2.5 days in the hospital and mostly immobile for a few days afterwards may have likely been the cause of some pain in the soles of both feet. I saw a foot doctor and slowly improved. I may have the name wrong - Plain Old Fascist? I don't think that's right, either.
Adaptations and challenges
The hospital stay
I studied the sheet of procedures and wanted to pack for the 3 days in the hospital. My only previous hospital experience was 1 night after going to the ER for what I thought would be just a couple of hours. Thinking I would go right back home after some tests and meds, I didn't pack or prepare for a hospital stay. So, I learned that I would rather take too much than not enough. For this shoulder surgery stay, I took extra clothes (totally unnecessary since I wore that disrespectful gown the entire time), toiletries (mouthwash or breath mints would have been enough), my daily pills, some collagen protein bars for afternoon snacks, all insurance cards, and an iPad, phone, and chargers. A friend brought me a bottle of cold brew coffee that the nurses kept in their refrigerator.
Took to hospital
• ID, insurance cards
• Pills: collagen, mints
• Cold brew: 1 bottle w/cream or 4 cans
• Deod, tthbrush, brush, mthwash, hairbrush
• Pad, phone, chargers
• Sling, Foot brace; Sox, sox, undies
At Hospital
• Request pain killer for first night.
• Wear sox, not leg tights.
• Wear ankle brace, exercise feet (no fascist)
• Sit to eat, stand up, walk halls
• Eat well: salmon & veggies, cold brew
Post-Op daily life
To prepare for having my right arm and hand out of commission for a while, I practiced performing routine tasks using only my left (non-dominant) hand. On the Monday before the Tuesday surgery, I spent most of the day with my right hand in my pocket. Here are some of the adaptations I made to ordinary tasks and routines:
For days before surgery, I practiced driving using only my left hand. Shifting gears, hitting the iPod buttons, turn signal, and even putting on the seat belt was all mastered while letting my right arm sit free on the console.
I practiced shaving with my left hand (good enough) and combing my hair (passable). Showering was tough since my right arm couldn't reach over to my left arm. Often I just took rinses instead of soapy showers. Fortunately, the weather cooperated by staying relatively cool. For deodorant, I bought one of the new sprays that don't leave a white residue or stain clothes. I got stumped at brushing my teeth. My left hand was not coordinated enough to make that easy. I mentioned my practice routines to a guy at the gym in the weeks before surgery and he suggested a battery powered electric toothbrush that I just had to hold, not stroke. Brilliant. Thanks to pocket computers and Amazon Prime, I researched and compared available options and had one ordered before he left the gym. It has worked well - I'll probly keep using it.
The first afternoon in the hospital there were crackers and Jello on my tray when I regained consciousness. I hadn't eaten since the day before so those were quickly gulped down. That evening, I ordered a meal of grilled salmon and grilled mixed veggies (it was very good). The food was delivered and placed on the bed tray in front of me. I just started laughing out loud. A nurse came in to check on me. I was so pleased that I had prepped and practiced life with just one hand, but it then hit me - I had never practiced how to eat with my left hand only. It just never occurred to me. Now I was hungry and faced with having to figure it out in a hurry. The salmon was easy to cut with the fork and the veggies were already bite-size.
Later, at home, I was eating an Atkins breakfast bowl and it kept sliding away from the spoon. I couldn't secure it with my other hand. I researched and Amazon Primed some sticky GelPads - the ones that hold your phone in place on your dashboard. They worked great to keep the bowl from sliding and turning while scooting food into the spoon. Later, for Surgery Part 2, I put pads on the countertop and on the tabletop. I could set jars on them and open the lids with one hand.



• Shorts with an elastic waist instead of a belt that requires 2 hands to operate.
• Sandals that can be slipped on easily. Later, when I wanted tennis shoes, I used ones with a one-handed lace clasp.
• Slick t-shirt that slid on and off easily, without having to move the right shoulder at all.
One of the Pre-Op directions I feared most was that I would have to sleep sitting up. I didn't think I could do that. But, the PA said I could sleep however was most comfortable (whew), but many people preferred elevating their shoulder by sleeping in a recliner or chair. I had researched lounge chair rental options. Instead, I just propped my slinged arm on a pillow and was able to sleep okay in the bed. I usually awoke after about 4-5 hours and, instead of stressing to go back to sleep, I would just get up - usually about 3am, have breakfast, and watch old sitcoms on TV. Some mornings I would go back to sleep from 5-7, my usual waking time. An afternoon nap helped ease the sleep deprivation.
On the first grocery shopping trip a considerate friend steered the cart, took the items off the shelf, put them in the cart, and carried my reusable bags to the car. Later, on my own, I would wheel the cart out to the car to transfer the bags into the car. Normally, I would grab the bags at the door and leave the cart in the cart corral in the store foyer.
What I wasn't prepared for was how lethargic, painful, and uncomfortable I would feel for the first week after surgery. I even felt too rotten to read a book. I had some guilt about not getting much 'work' done. For surgery Part 2, I was better prepared - I watched tv, worked puzzles, built Lego, and rested.
To minimize time away from normal activities, and speed up recovery and rehab. I researched a variety of options and procedures. The result was the factors listed below. As before surgery, I was going to Physical Therapy regularly. The first session after surgery was to test the shoulder's range of motion. The PT measured angles of the arm up and to the sides. He finished his assessment, turned to me and said, well, you've already achieved the results we would have done in several weeks of motion therapy. You won't need to come back until we start strength exercises. I asked if I could start them now. He said, no, the shoulder still needs time to heal. So, I started the strength exercises at the gym. I set the weight to zero and started with micromovements to strengthen muscle and increase blood flow. The Physical Therapist, Surgeon and Physician's Assistant all expressed surprise and admiration at how fast and how well I was recovering.
I attribute the faster-than-normal recovery to these factors
• Positive attitude - from pre-surgery through rehab.
• Good nutrition - higher protein, vitamins, less sugar and fewer carbs.
• Collagen protein is the 'glue' that holds us together, makes up about 30% of all body proteins - tendons, ligaments, bones, skin, and hair.
• Healing Elixir - I drink a smoothie every day, starting about a week before surgery and continuing to now.
• Clean and sober: no alcohol, no drugs, minimal prescription drugs; allowed my brain to be more in tune with my physical needs.
• Trust my body - respected its pain and comfort; trusted my experience, wisdom, and common sense; took doctors instructions as guidelines, not requirements.
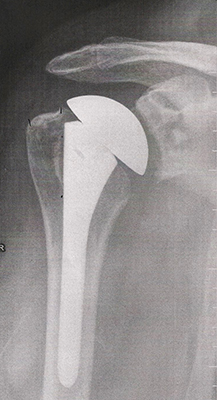
• Exercises - performed full sets of rehab routines at the gym, 3 days/week.
• Prepared for accommodations and limitations in advance.
• Oxytocin increases following intense social interaction have been correlated with reduction of inflammation, thus allowing a wound to heal more quickly.
• Stem cells - millions of young, fresh, eager-to-help cells throughout my body.

Healing Elixir ingredients
1. Collagen Protein.
2. Green Juice; Superfood nutrient powder.
3. Tart Cherry juice; comparable anti-inflammatory activity to ibuprofen and naproxen, but without side effects.
4. Yogurt - sugar-free, fruit flavor.
5. Sugar-free non-dairy creamer - to make a thicker smoothie.
6. Dash of cinnamon.
7. Sugar-free ginger ale.
8. Ice.
ACCESSORIES FOR MEDICAL ARM SLINGS
During a recent stay in the hospital for a total shoulder replacement, I boarded my dog Brooklyn at her favorite dog daycare. The next morning, after bringing her back home, I resumed the schedule of walking her each morning and evening. But, I couldn't reach my phone/palm computer in my pants pocket. First, I put my phone in my other pocket, but it had to share space with the stuff in that pocket. Later, I simply stuffed my phone in between the sling and my arm. Not bad, but I worried about it falling out. I then remembered that I had an unused pouch - I added velcro to the back. It stuck easily to the outside of the sling and worked well as a carry-all. Then I realized I could also attach a cup holder to the flat top of the pillow on the inside of the sling. This had possibilities.
I further explored and determined carrying needs and solutions. The prototype items worked great - functional, not too obtrusive, and respectful of the black sling. Cups and bottles in the cup holder were quite secure and the pouch was big enough to hold my phone, energy bars, and snacks. Google searches showed nothing on the market for attaching items to medical slings. I showed my nurse neighbors who loved the idea and saw numerous possibilities. When I showed the Physician Assistant - I was curious if he had seen the idea before - he also loved it and commented that he had never seen such products. Also got positive feedback from Physical Therapists.


Any combination of Accessories can be velcro attached to the various parts of the arm sling - they help the user to live a more normal and more active life - able to carry items one normally might while hiking, walking the dog, shopping, exercising, going to movies. It's not just a sling - it's a Carry-all!
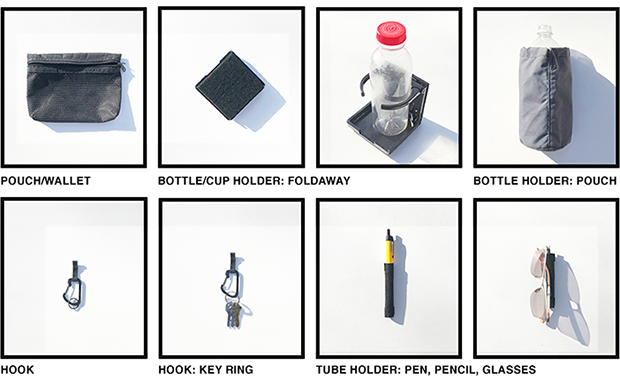
ACCESSORIES
• Pouch/Wallet: to hold smartphone, music player, ear buds, TV remote, snacks, sunglasses.
• Bottle/Cup Holder, collapsible/fold-away style or Pouch style
• Hook: caribiner for keys and hanging items.
• Tube Holder: for pen, pencil, eyeglasses.
TARGET AUDIENCE
Any teen or adult who wears a sling and has a desire or need to conveniently carry items. Would likely be ordered online while ordering the sling or offered by Orthopedists, Physicians Assistants, Nurses, Physical Therapists, and Athletic Trainers.
OBJECTIVES FOR SLING ACCESSORIES
• Solid material (not mesh), to provide privacy of stored objects.
• Black, to be discrete on black slings and straps.
• Lightweight, to not add stress on the neck.
• Pouch: minimal bulk, but large enough to hold smartphone.
• Easy to access pouch contents, velcro tab (no zippers).
• Easy to attach and remove from a sling, using one hand only; tabs of velcro on each accessory.
• Secure attachment, to firmly support contents.
DATES
• Inspiration: Friday, September 8, 2017
• Built prototypes and tested: September 8-10
• Wrote and posted Sling Accessories webpage: Thursday, September 14
• Bought pouch at Cabela's: Saturday, September 16
• Ordered black cup holder on Amazon: Sunday, September 17
• Met with Patent Attorney: Friday, November 10

For Surgery Part 2, I had just returned from Walt Disney World and added pins of Mickey and Chip & Dale.
May 2019: I like your sling that you invented. Is it on the market yet? My sister had a stroke and lost the use of her right arm, this would be great for her so she could carry stuff she needs to at least make that arm useful again while hanging in a sling. Please let me know where and when I can purchase one.
It is a monster idea and I would have been a buyer. Thank you for pointing me in a direction to put one together for her. Good luck on your other ideas. Hope you have great success!
Kneess
Patella Tendonitis
Knee pain while walking Brooklyn in the morning.
Diagnosed: Febuary 27, 2023
Flat walks, strap, exercises.
Painless: March 6

Knee diary
Jan 2025
17 Lateral pain: pain 6
23 Leg press pain: pain 8
Febuary
1-5 None, no discomfort
6 None, less fatigue
7 None, gym
8- 2/3 pain
March
No pain, no discomfort
28: lateral wrench, pain
Meloxicam
Voltaren
Additional Aleve
Steroid shots
2024: Jan 1, April 1, July 1, Oct 1
2025: Jan 3, April 3
Get pain episode: pain pill, voltaren
Swelling: make appt
Assess: April
Knee notes
Steroid every 3 months
If stiff: ride bike
Gym: low weight, 20+ reps
Voltaren as needed
Knee/patella brace as needed
Back
Feb 10, got worse daily
Thurs/Fri March 6-7: 2-8/9
Sat March 8: okay am; 4p: 8/9
start Aleve: 10a 6p
Sun 9: a 8/9, n 3 / 8
Mon 10: a 8/9
Tues 11: worst day yet
Wens 12: doctor: steroid shot, up aleve, start muscle relaxer
Fri 14: better
Aleve: full stomach, 2 morning, 2 evening
Flexor muscle relaxer: 1 evening, add 1 am if needed
Ease into exercises when ready
Call if symptoms maintain or get worse
Scoliosis
X-rays: September 20, 2023


Bladder implant
November 6-9: Axonics trial device: failed

www.jamesrobertwatson.com/shoulder.html